By Manya Goldstein
Our modern food landscape is spectacular, isn’t it? Walk into the average grocery store, and it appears as if you’ve entered food nirvana. The aisles overflow with a dizzying array of items, from Oreos and Cheez-its to Kashi and Greek yogurt. The products call out from their home on the shelves, singing masterfully-tailored appeals to entice each kind of consumer. Some might be captured by the mouthwatering packaging, others by the impressive health claims… and for a number of us, it’s simply the memory of a taste we just need to experience again.
There was a time, not too long ago, when the food we ate did not come in a package. Labels were non-existent, as were the complex ingredient lists we’re accustomed to today. We simply cooked and ate real food. Yet those days are gone, replaced by the industrial food complex that has embedded itself into the very fabric of American life. Our processed food products — our chips and granola bars and hummus packs — are just so convenient, so affordable and so pleasurable that most people can’t imagine life without them.
More than 60 percent of the American diet consists of highly processed foods — foods that have been taken apart and put back together again with various combinations of sugar, salt, oil and additives. It’s no surprise that junk food and frozen dinners fall into this category, but many innocent-looking kitchen staples do as well. For instance, the majority of industrially-produced breads are intricate concoctions of refined grains, sugars, emulsifiers, dough conditioners and preservatives. Oh, and we can’t forget the synthetic vitamins added back in to make up for the nutrients stripped away during processing.
Two years ago, I didn’t think twice about what I ate. Taste and convenience guided my food choices above all else. Like most Americans, I thought orange juice and granola bars were healthy. In fact, I really knew nothing about nutrition except the adage that fruits and vegetables are good for you. And why would I think twice about food? I felt fine. No one ever told me to eat differently. And besides, everyone else was doing the exact same thing.
Quite simply, I was in for a rude awakening. Just one month after I entered college, I came down with a host of frightening symptoms that began with near-fainting spells and progressed into a slow breakdown of my autonomic nervous system. This is the system responsible for basically everything our bodies do without our conscious control: heart rate, digestion, breathing, temperature regulation… you name it. I was diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS), a condition characterized by an excessive jump in heart rate upon standing that really just means your autonomic nervous system can’t regulate circulation (and usually many other of its necessary jobs).
The independence coveted by the average college kid took on an entirely new meaning for me. I travelled from doctor to doctor desperately trying to get my symptoms under control. Most offered me a handful of drugs, which I gladly accepted. The more knowledgeable ones told me to increase my salt and fluid intake to expand blood volume, exercise to improve vascular tone and buy compression garments to help circulation. But nothing worked. I hit rock bottom the summer after my freshman year when I began having week-long crashes of total nervous system shutdown. I couldn’t stand, walk, breathe well, digest or even think. I felt like a half-conscious shell of my former self, and no one knew what to do.
By the time a family friend recommended I see a holistic specialist, I was willing to try anything. I walked through the clinic doors with no idea what to expect and soon found myself standing in an entirely new world of knowledge. The specialist spoke about the body as an interconnected system, influenced by everything from the food we eat to the lifestyle we lead…
Wait, what? Back up a second. Our food choices can’t really matter that much,I thought.
I mean, c’mon, it’s just food. And besides, I have a nervous system problem. The doctors gave me a diagnosis; they say its chronic. I’m just trying to control my symptoms a little better. That’s the end of the story.
Looking back, this was a completely normal response for someone growing up in conventional American society, eating conventional American food and seeing conventional American doctors. No one talks about the environmental factors that influence disease, most notably the chronic conditions that dominate today’s health landscape. We treat illness as an isolated problem with a corresponding black-and-white solution. You have depression? “Here is an anti-depressant.” You have Crohn’s? “Your immune system is overactive. We’ll have to control it with immunosuppressants.”
With chronic conditions ranging from asthma to allergies to arthritis, there’s rarely any talk of “Why is this happening?” and certainly no discussion of “How can we reverse it?”
Therefore, it is only natural to react with disbelief — and often rejection — when introduced to this entirely new paradigm of thinking about disease.
And that’s just what I did.
It took me a solid six months of seeing the holistic specialist to accept the fact that my everyday food choices directly affect my health. When people would ask me about POTS, I told them about the holistic approach I was pursuing. “I mean it makes sense that our food and environment affect us,” I would say. But for a long time, this was a half-hearted declaration, one that I did not entirely understand or believe myself.
Even once I started researching for this project, it took me months to internalize that food has well-established links to the leading chronic diseases plaguing society, diseases like heart disease, cancer, Alzheimer’s and diabetes that are responsible for 7 out of 10 deaths in America — and worldwide according to a new Lancet study.
The study was published ahead of a Sept. 27 meeting at the United Nations General Assembly, which brought 500 experts together to discuss the chronic disease epidemic. Speakers repeatedly called for action, declaring that 41 million people die each year from preventable conditions.
In fact, research shows that diet is the top risk factor for mortality in our country.
What?! I simply couldn’t believe that this was the case. Why don’t more people know how much food matters? Why don’t doctors talk about it? And most importantly, why aren’t we doing anything to fix it?
But let’s not get ahead of ourselves with too many questions. I’d like to return to the grocery store to unpack what’s really wrong with all of the processed food I grew up with — the food that simply seemed too tasty and convenient to live without.
Part I: Unpacking Processed Food
So what’s really wrong with processed food? I mean c’mon, it’s just food. It can’t be that bad (i.e. Please don’t take away my Oreos!)
The sad answer to that question is, well, almost everything.
Let’s start at the very beginning with an ingredient so prized by the food industry that they add it to 74 percent of their products. It’s something that practically symbolizes childhood, something so soothing and sweet that we can always rely on it when we need a friend.
Yup, you guessed it. It’s sugar.
Sugar is magical — not only to children but to the food industry as well. We all know that sugar makes things sweet. But did you know that sugar can enhance the flavor of savory foods? It can also retain moisture, improve texture and act as a preservative, among a number of other impressive feats.
The classic line is that sugar is “empty calories,” but an increasing number of experts are arguing that sugar’s calories are far from empty.
“Sugar is metabolized in the liver virtually identically to alcohol,” said Dr. Robert Lustig, a neuroendocrinologist and professor of pediatrics at the University of California San Francisco.
Wait. Sugar is the same as alcohol?! We know alcohol is bad. We would never give alcohol to kids, but we give sugar to them all the time thinking it is harmless. How could this possibly be true?
We’ll get there, but first we need a brief biochemistry lesson to explain the sugar hypothesis.
Sugar is a type of carbohydrate called sucrose. Sucrose is made up of two components: glucose and fructose. When we eat sugar, it gets broken down into these two components. With me so far?
Great, so the glucose can be metabolized by all organs. That’s all that’s important for now. The fructose, on the other hand, must be processed by the liver. Now, the liver can handle fructose in small doses, such as the fructose that trickles in from a fiber-packed orange. But the concentrated hit of fructose from sugar simply overwhelms its capabilities. The liver metabolizes as much as it can, but it has no choice to convert the rest to fat. The fat builds up around the liver, which impairs its functioning and leads to insulin resistance. It also gets transported out into the blood, increasing visceral fat (the fat in our abdominal cavity) and our cardiovascular risk. Collectively, this cycle is known as metabolic syndrome, and it sets us up for a multitude of problems — including those previously confined to adulthood.
“There are two diseases that children never got before: Type II diabetes and fatty liver disease,” Lustig said. “Prior to 1975, those two diseases were the diseases of aging and the diseases of alcohol. Now kids get them.”
How exactly do children get the diseases of alcohol without consuming alcohol? According to Lustig, the answer is clear: sugar.
The sugar hypothesis states that sugar causes insulin resistance, which many experts believe lies at the heart of our chronic disease epidemic. Insulin is the fat-storage hormone released when we consume carbohydrates. It pulls glucose out of the blood and into our cells, keeping our blood sugar stable. When we stop responding to insulin, it sets off a cascade of detrimental consequences throughout our bodies.
“We have an epidemic of insulin resistance, and it manifests itself as obesity and diabetes and heart disease and cancer and Alzheimer’s and strokes. This is the paradigmatic disease of Western diets and lifestyles,” said Gary Taubes, an investigative science journalist and author of “The Case Against Sugar.”
Lustig and Taubes are among a new school of experts working to combat the message that “a calorie is a calorie.” According to this logic, obesity and related conditions such as diabetes stem from an energy balance problem: too many calories in, not enough calories out.
The food industry loves to promote the calorie hypothesis to mitigate criticism. (In Lustig’s words, “Don’t blame our calories; go blame somebody else’s calories.”) However, the notion also remains entrenched in the professional realm of nutrition.
“The world is full of ‘scientists’ who clearly believe a calorie is a calorie. I’d say 99 percent of the community thinks that it’s all about energy balance. ” Taubes said. “Clearly, the energy balance story was the sugar industry’s best friend — the gift that keeps on giving. But had the scientists done their job, they would have just dealt with it.”
In their argument against the calorie hypothesis, Lustig and Taubes explain that calories are metabolized differently in the body depending on where they come from, and certain calories can make you sick regardless of whether you are overweight. In fact, up to 40 percent of normal-weight people have metabolic dysfunction, and 20 percent of obese people are healthy.
“What really bothers me is that I majored in nutrition and food science in college back in the 1970s, and I knew about nutritional biochemistry and that different foods were metabolized in the body differently,” Lustig said. “Then I went to medical school, where they beat it out of me. They said, ‘It’s only about calories’. I actually practiced that way for the first 20 years of my career, and then I started doing the research to show that that actually isn’t true.”
As it turns out, not all calories are created equal — and it appears sugar may be the most harmful.
“Sugar’s not dangerous because of its calories or because it makes you fat. Sugar is dangerous because it’s sugar. It’s not nutrition. When consumed in excess, it’s a toxin. And it’s addictive,” Lustig writes in his latest book, “The Hacking of the American Mind.”
Sugar In the Brain
People may joke that they’re addicted to chocolate or other sweets, but there is actually research to back it up.
When we eat sugar, it activates the brain’s reward system and causes dopamine — the pleasure neurotransmitter — to rise. Neuroscientist Dr. Nicole Avena explains that it’s normal for dopamine to be released when we eat new foods; it’s an evolutionary mechanism that helps us pay extra attention to determine if a food is safe. However, the dopamine response should subside after repeated exposure to the food.

Sugar, on the other hand, plays by different rules.
“Dopamine is released in response to a sugar binge even when sugar is no longer a novel food. It is as if the brain starts to treat sugar like a drug,” Avena writes in her book, “Why Diets Fail,” co-authored by John Talbott.
The biochemical reaction is so strong, it may be almost impossible to resist sugar’s call. Rats will run across an electric grid to reach M&M’s. They will even choose sugar over cocaine when they are already hooked on the powerful stimulant.
In its natural form, sugar is not addictive. Besides, it only exists naturally bound up with fiber in fruits and some vegetables or as honey guarded by bees. As Lustig and his colleagues put it, “Nature made sugar hard to get; man made it easy.”
Only after sugar is refined does its addictive potential become fully actualized, not unlike other drugs.
“Indeed, when sugar cane is crushed and drained of all its liquid contents, boiled down to a syrup, shaken and then stripped of all its vitamins, minerals and molasses, we are left with pure white crystals. This extraction and refinement process is similar to that of other addictive white crystals, that is, cocaine from the coca leaf, and opium from the poppy seed/pod,” Dr. James DiNicolantonio and colleagues write in a 2017 paper, “Sugar addiction: Is it real?”
And like these other “white crystals,” we can build up tolerance to sugar as our dopamine receptors downregulate, requiring more input to feel the same reward. So that one piece of chocolate really might not be enough.
Given sugar’s addictive properties, some experts argue that it might be almost impossible to moderate our intake.
“Trying to consume sugar in moderation, however it’s defined, in a world in which substantial sugar consumption is the norm and virtually unavoidable, is likely to be no more successful for some of us than trying to smoke cigarettes in moderation — just a few a day, rather than a whole pack,” Taubes writes in The Guardian.
Safety First
But let’s put sugar’s addictive potential aside for a moment. How much sugar is safe to eat?
Though the American Heart Association is not always known to give the best dietary advice due to conflicts of interest — don’t worry, we’ll get to them later — their sugar limits are a good place to start.
The AHA recommends that men consume no more than 9 teaspoons of added sugar per day, and women consume no more than 6 teaspoons. For children, the range is 3–6 teaspoons depending on their size.
Let’s put that in perspective. A 12-ounce can of Coke contains 39 grams of sugar, which is equivalent to 9.75 teaspoons. So if you have a standard-sized soda, you’re already over your daily allotment. Don’t even think about that Big Gulp.
Sugar is listed on nutrition labels as grams, but seriously who can visualize that?! To convert grams to teaspoons, simply divide by four.
And remember, sugar is added to 74 percent of processed foods, even products marketed as healthy.
For instance, Tazo’s organic chai latte contains 6 teaspoons of added sugar. Perhaps you’d like to enjoy it with a serving of Chobani strawberry greek yogurt, which has 4.5 teaspoons of its own. It may sound like a healthy snack, but you’d already be well over your daily limit. Sugar sure adds up fast, no?
In middle school, I used to trade my Oreos for a friend’s LUNA bar — not for health reasons per se, but I thought the protein bars were healthy enough that they became my lunch staple for the next five years. It turns out that LUNA bars contain the same amount of sugar as three Oreos. I should have just kept the cookies.
Perhaps the most surprising fact: 12 ounces of orange juice is equivalent to over 8 teaspoons of added sugar even though all of the sugar is natural. Why? Juice lacks the essential fiber that eases sugar’s bombardment of the liver.
Food manufacturers excel at disguising sugar in their products. There are at least 61 names for sugar, from rice malt to dextrose to dehydrated cane juice. Why go to all this trouble? Because ingredients lists are sorted by weight. Even if consumers don’t understand how sugar affects their biochemistry, they might become wary if sugar is the first ingredient.
To add to the confusion, manufacturers were not required to list added sugars or their percent daily value on nutrition labels in America until this year. The sugar industry naturally wasn’t thrilled with the decision, claiming it was based on “inadequate scientific evidence.” Many products still do not feature the updated labels, and it’s no mystery why companies are stalling.
When we combine misleading packaging with sugar’s addictive potential — and its ubiquity in food products — it’s no wonder that the average American consumes 19.5 teaspoons of sugar per day, nearly 300 percent more than we should.
The Woes of Refining
Though sugar is a big problem in the world of processed food (some would argue the biggest problem), there are many other areas of concern worth our attention.

Highly refined grains serve as the foundation of most processed food items. Not only does the refining process improve the shelf life of products, it also enhances texture and appearance (think of white bread). In doing so, however, it strips grains of essential fiber and nutrients.
Food manufacturers are well aware of this, and so they add a handful of synthetic B vitamins and iron back in after processing. In fact, the USDA tells consumers, “Check the ingredient list on refined grain products to make sure that the word ‘enriched’ is included in the grain name.”
The problem is that food is more than a few vitamins thrown together.
“A whole food is a matrix of all these compounds and nutrients and minerals and vitamins — thousands of substances that interact with each other,” said Kristin Lawless, a journalist and nutrition consultant who recently published “Formerly Known as Food.” “If you add a synthetic vitamin to, say, refined white flour, it is not going to be as readily absorbed by the body or utilized in the same way as if you ate the whole grain.”
The loss of fiber in the refining process is perhaps even more problematic because it cannot be added back in (though that doesn’t stop some food companies from trying).
There are two primary types of fiber: soluble and insoluble. As Lustig explains in his 2013 book “Fat Chance,” the two work together to form a “gelatinous barrier” along our gut to slow the absorption of food. Just like the fiber in fruit slows the rate of fructose hitting our liver, it also delays the absorption of glucose, which in turn lowers our body’s insulin response. By regularly consuming refined carbohydrates, we put our bodies on an insulin roller coaster and set ourselves up for cravings, weight gain and metabolic distress.
(Experts debate whether the primary driver of metabolic dysfunction is sugar or sugar plus other refined carbohydrates. Clearly, more research must be done, but our best bet for now is to limit both.)
But fiber is crucial for another reason: to feed our gut bacteria. Our gastrointestinal tract houses trillions of microorganisms that are collectively known as the “gut microbiota.” They play a critical role in maintaining our health, one that researchers are just beginning to understand. What we do know is that low bacterial diversity has links to a range of health problems from autoimmune diseases to inflammatory conditions, as Dr. Ana Valdes and colleagues outline in the British Medical Journal. We also know that a flourishing, diverse gut microbiota requires fiber. Low-fiber diets have been shown to reduce species diversity, which can potentially worsen from generation to generation.
“Fiber is probably the single most important factor driving the microbiota and health,” said Maria Gloria Dominguez-Bello, a Rutgers University professor of microbiome and health and fellow of the American Academy of Microbiology. “If we don’t eat enough fiber, we starve our gut microbes.”
When we starve our gut microbes, many bacterial populations die off and we’re left with lower species diversity. But it gets worse — the microbes that do remain must eat their only available source of food: our intestinal lining.
“When you starve the colon, the only microbes that can survive are those that attach to our epithelium and feed on us, including mucus degraders,” Dominguez-Bello said.
The mucus-protected epithelium serves as an important barrier to keep our bacteria away from the intestinal wall. When mucus-degrading bacteria start feasting on it, our immune system goes on hyperdrive, resulting in chronic inflammation that can also contribute to the progression of disease.
If we don’t feed our body right, it will quite literally eat us.
The bottom line is that real food is high in fiber. Processed food is not. Real food is chemically diverse (and thus drives a diverse microbiota). Processed food is not.
However, our processed food landscape gives us the illusion of diversity. Grocery stores are filled with countless variations of breads, pastas, snacks and desserts. Though they appear different on the outside, these products are largely variations of the same raw materials dominated by corn, soy, wheat, sugar and vegetable oils.
“All of these foods are chemically similar, but sensorally they are not,” Dominguez-Bello said.
In other words, our senses tell us that we are eating a variety of foods. It appears as if our options are endless when we walk through the grocery store aisles. But at the end of the day, it is all an illusion — one that the food industry excels at creating.
Greasy Business
Apart from sugar and refined grains, vegetable oils represent another fundamental pillar of the processed food industry. For years, we’ve been told that vegetable oils are a healthier choice than saturated fat, which was said to cause heart disease. Though we now know that saturated fat has no connection to cardiovascular risk, the dogma became so embedded in the public health community that it is still echoed to this day. (Don’t worry, we’ll fully examine the fat debacle later on.)

Vegetable oils are highly processed oils extracted from seeds such as corn, rapeseed, sunflower and, most notably, soybeans. According to food author Michael Pollan, 75 percent of the vegetable oils we consume are derived from soy.
But making vegetable oils is no easy task. Seeds are quite different than olives which “ooze with oil,” as Melanie Warner writes in “Pandora’s Lunchbox.” In fact, she refers to soybean oil as a “complex, high tech product” before outlining the lengthy process it entails.
To extract the oil, manufacturers use a harsh chemical solvent known as hexane. (Indeed, Warner explains that it is so harsh, factories must be explosion proof.) The oil is then treated with more chemicals, bleached and deodorized at 500° degrees. But that’s the short version.
As Warner writes: “At long last, after multiple rounds of heating, chemical treating, centrifuging, filtering, washing, and vacuuming, the soybean oil — clear, odorless, nearly nutrient-free — is edible, ready to be pumped into eight-thousand-gallon tanker trucks and shipped off to customers across the food industry.”
This process results in a highly unstable oil, which was not very stable to begin with since it is a polyunsaturated fat. From a chemistry perspective, polyunsaturated fats oxidize much faster than saturated or monounsaturated fats since they contain multiple double bonds.
“Each bond provides an additional opportunity for the fatty acid to react with the air, so the oils oxidize — and go bad quickly,” science journalist Nina Teicholz writes in “The Big Fat Surprise.”
Alright, so we know that vegetable oils are quite fragile, to say the least. What happens when we add heat to the mix? According to researchers, the picture gets ugly very quickly.
“Heat degrades polyunsaturated fatty acids to toxic compounds,” De Montfort University professor Martin Grootveld and colleagues state in a report published in Foodservice Research International. According to the report, the toxic oxidation products may lead to a number of problems ranging from birth defects to cancer.
In restaurants, oxidation products emitted from the fryers’ mist build up as “thick gunk” on all cold surfaces, Teicholz writes. The toxic compounds are so unstable, she says worker uniforms have been known to “spontaneously combust” in the dryer.
Vegetable oils don’t seem so innocent after all.
As if that’s not enough, this processed food staple poses another problem: they throw off our omega-3 to omega-6 balance.
Omega-3 and omega-6 are essential fatty acids that have historically existed in a 1:1 ratio. The ratio is now 20:1 or higher thanks to changes in diet, most notably our increased consumption of vegetable oils rich in omega-6 fats.
But why does this matter? Experts say that a skewed fatty acid ratio can promote inflammation throughout our bodies.
“The imbalance between these two types of fatty acids will push us toward a pro-inflammatory state,” said Todd Robinson, a naturopathic doctor and owner of Wellness Working Group.
He explains that a diet filled with whole foods — like fish and vegetables and nuts — tends to be omega-3 rich, whereas the standard American processed food diet tends to be omega-3 poor. At the same time, our modern diet provides a hefty dose of omega-6’s, pushing our ratio toward the pro-inflammatory side.
“As with most areas in biologic systems, it’s about the balance,” Robinson said. “We are supposed to mount an inflammatory response if we get injured; that’s part of how our body heals. The problem is chronic, unchecked inflammation, which contributes to conditions like heart disease and dementia and diabetes. If people eat a diet that helps their bodies maintain a natural inflammatory balance, they are going to be healthier in the long run.”
Adding or Subtracting?
Whenever I make a passing comment about food safety, I almost always receive a variation of this response: “Oh, I’m not worried, I’m sure there are regulations.” Unfortunately, our sense of security turns out to be misplaced.
There are over 10,000 substances directly or indirectly added to our food, according to a 2011 report led by chemical engineer Thomas Neltner. Direct food additives include everything from emulsifiers and preservatives to colors and flavorings. The food industry relies on them to keep products fresh, consistent and appealing to both our eyes and taste buds. Indirect additives are the substances that come into contact with our food during processing and packaging, such as plastics and lubricating oils. They do not have to be listed on labels, though they can leach into food.

Most people are unaware that the Food and Drug Administration does not perform safety testing. Rather, the companies themselves are responsible for assessing the safety of their products.
“The manufacturers are the ones doing the safety testing in their own laboratories with their own hired scientists,” journalist and nutrition consultant Kristin Lawless said.
To top it off, the system is entirely voluntary. If companies don’t want to notify the FDA about their ingredients, they have no legal obligation to do so.
“The chief problem with the food-additive self-regulation is that it provides no incentive for either the industry or the government to do — or even to review — the difficult and often expensive studies that might result in bad news,” Warner writes in “Pandora’s Lunchbox.”
So when researchers dug deeper into the data on food additives, it’s no surprise the results were concerning. One evaluation found that most additives in our food supply have not been adequately tested for safety.
“Almost two-thirds of chemical additives appear to have been declared safe for use in food without the benefit of being fed to an animal in a controlled toxicology study,” the researchers state in a 2013 paper published in Reproductive Toxicology.
Even if all food additives were properly tested for safety, it still doesn’t take into consideration cumulative or synergistic effects. We rarely consume additives in isolation; rather, we receive a diverse chemical cocktail when we eat processed foods. According to the American Academy of Pediatrics, chemical exposures can interact with each other and interfere with similar biological pathways. Therefore, it is crucial for regulators to take these considerations into account.
So far, we’ve examined a number of problems with processed food — from the sugar to the lack of fiber and nutrients, from the vegetable oils to the chemical additives. Still, one question remains: How did we get here? If processed food is so bad for us, how did it take over America’s eating culture?
Part II: Processed Food Takeover
Given the thousands of products in our grocery stores, it might be hard to believe that processed food is a relatively new phenomenon. Its story goes back to the early 1900s, but it didn’t truly take off until post-World War II when the food industry began persuading women to forgo traditional cooking.
“The food industry launched this huge campaign to get women to bring their products into the home,” Lawless said. “They were marketed as ‘liberation for women!’ and ‘freedom from the kitchen!’”
In “Pandora’s Lunchbox,” Warner describes how the industry’s advertising tactics were not immediately successful. Yet within a decade, their “exhortations to abandon the kitchen” took hold and industrial food started to change our entire way of eating.
“They became part of a family tradition in place of traditional whole-food cooking,” Lawless said. “The industry embedded their products into the culture, into the home and made them completely normalized.”
As technology expanded, traditional marketing gave way to more advanced tactics to further embed industrial food into our lives.
In his exposé “Salt, Sugar, Fat,” Michael Moss outlines how today’s food manufacturers capitalize on the latest science to enhance the appeal of their products. He describes how companies hire highly-trained food scientists to calculate the “bliss point” of sugar and manufacture the perfect “mouth feel” to optimize the “crave-ability” of their products. (They avoid the term “addictive” like the plague.)
Moss writes: “[The products] are knowingly designed — engineered is the better word — to maximize their allure. Their packaging is tailored to excite our kids. Their advertising uses every psychological trick to overcome any logical arguments we might have for passing the product by. Their taste is so powerful, we remember it from the last time we walked down the aisle and succumbed, snatching them up. And above all, their formulas are calculated and perfected by scientists who know very well what they are doing.”

Surprisingly, federal policies also helped to facilitate the takeover of processed food by subsidizing the food industry’s main ingredients — most notably, corn and soy.
“The business model of the food industry is organized around ‘adding value’ to cheap raw materials; its genius has been to figure out how to break these two big seeds down into their chemical building blocks and then reassemble them in myriad packaged food products,” Michael Pollan writes in his 2008 book, “In Defense of Food.”
We’ve already mentioned that 75 percent of our vegetable oils come from soy, but so do a myriad of food additives from thickeners to stabilizers (think of soy lecithin that is found in most chocolates). Along the same token, Pollan writes that more than half of our sweeteners come from corn. Corn can also be broken down into its own bundle of additives including emulsifiers, flavorings and even synthetic vitamins.
“Products infused with corn and soy additives line our grocery and pantry shelves — breakfast cereals, baked goods, candy, frozen desserts, ketchup, dressings and sauces are a few household favorites,” researchers write in a 2013 U.S. Public Interest Research Group report.
The report states that crop subsidies favor “junk food production” over fruits and vegetables, which receive only one percent of federal payments. To illustrate, the authors directly compared apples to a timeless American processed food item: the Twinkie.
“Of the 37 ingredients in a Twinkie, taxpayers subsidize at least 17, including corn syrup, high fructose corn syrup, vegetable shortening and cornstarch.”
If the money had gone directly to taxpayers, the authors calculated that the apple subsidies would enable each person to buy half an apple each year. Yet they could afford almost 20 Twinkies with their junk food subsidies.
“Rather than reflecting our nation’s established health priorities, these subsidies mirror a pattern of special interest influence. With childhood obesity rates worryingly high, this use of taxpayer dollars thwarts common sense. Almost any other conceivable use would be a wiser investment,” the report concludes.
Yet despite all of these factors, we have to dig a bit deeper to fully understand the takeover of processed food. Besides, doctors and public health officials should have eventually caught onto the health risks and started speaking out against the food industry and federal policies. Why didn’t this happen?
Industry and Institutions
The food industry has not only managed to embed itself into consumers’ lives but into the professional health realm as well.
The Academy of Nutrition and Dietetics (AND) is the world’s largest association of nutrition professionals. They claim to be “committed to improving the nation’s health and advancing the profession of dietetics through research, education and advocacy.” However, according to a 2013 report by public health lawyer Michele Simons, the AND boasts nearly 40 food industry sponsors that include Coca-Cola, PepsiCo, Kellogg, Mars and General Mills.
The industry sponsors run many programs, including continuing education courses for dietitians. The problem is that the food industry is not “in the education business,” as Simon puts it. “It’s in the selling-more-food business.”
Therefore, companies hire seemingly credible experts to teach biased material that supports their aims. Simons described a Coca-Cola webinar taught by a Harvard professor who attempted to neutralize concerns about sugar, calling them “urban myths.”
Hershey sponsored another continuing education opportunity that brought nutrition professionals to their Pennsylvania headquarters for a full-day workshop.
“To cover up the fact that nutrition professionals were visiting a candy store, the event was called ‘From Nature to Nutrition: A Hands-on Exploration of Natural Cocoa from the Bean to Health Benefits,’ and was listed in the program as ‘Planned with Academy Partner: Hershey Center for Health & Nutrition,’” Simons writes.
The AND’s deep corporate ties are perhaps best illustrated at the organization’s annual expo. Though more than 300 vendors attend the event, Simon says junk food companies dominate the floor.
“It’s a truly surreal experience just to walk into the expo hall,” she writes. “You know it’s supposed to be a nutrition conference and yet it feels like a food industry event. Junk food expo is really the best descriptor.”
Industry even influences science itself. Science journalist Nina Teicholz explained to me how the food and pharmaceutical industries fund university scientists and departments, underwrite scholarships, endow chairs, sponsor conferences…and the list goes on.
“It’s pretty much endless,” she said.
In her research, Teicholz has found that the largest influence comes from the vegetable oil industry. In fact, there has only been one conference dedicated to the potential harms of vegetable oils, despite the mounting evidence against them, because no one will sponsor the topic.
“If there is no conference to bring people together, if there are no conversations, there is no air for an idea to breathe and grow,” she said.
What’s more, the vegetable oil industry practically launched the American Heart Association (AHA) itself. Teicholz said the office of cardiologists remained small and underfunded until 1948. (Besides, cardiology was a new profession since heart disease had been quite rare until a few decades before.) She explained how Procter & Gamble, the inventor of vegetable oils, changed everything when they chose the AHA to be the beneficiary of their popular radio contest.
“The American Heart Association, in their official biography, writes that millions of dollars flowed into their coffers and they were transformed practically overnight into the national powerhouse that they are today, opening offices across the country and really becoming a force in public health,” Teicholz said.
Procter & Gamble continued to support the association (along with many other food giants). Then in 1961, the AHA became the first group in the world to recommend that we limit saturated fat and cholesterol — and consume vegetable oils instead.
Teicholz emphasizes that we should not solely blame industry for this very misguided nutrition advice. Rather, our demonization of fat stems from scientists who fervently believed it drives heart disease.
It all began in the 1950s when University of Minnesota physiologist Ancel Keys drew a simple line of causation from the fat we eat to the cholesterol in our blood to heart disease, thus becoming the father of the diet-heart hypothesis.
“This connect-the-dot exercise in 1952 was the acorn that grew into the giant oak tree of our mistrust of fat today,” Teicholz writes in her book “Big Fat Surprise.”
Keys’ hypothesis was just an idea, yet it became accepted as truth before being properly tested in clinical trials. Once the diet-heart hypothesis became institutionalized by the American Heart Association and the National Institute of Health, Teicholz said it became almost impossible to change.
“Scientific institutionalization is almost an oxymoron,” she said. “Science requires that one be self-doubting, nimble, able to change according to new scientific observations. Institutions require just the opposite: they require constancy to not lose the faith of the public.”
So despite the fact that billions of dollars of research over the following decades could not prove the diet-heart hypothesis, it remained entrenched in dietary policy and the minds of countless scientists.
“The idea, like DNA, has been carried from one generation to the next of scientists who have committed their entire careers to those beliefs,” Teicholz said. “The critics were silenced, and the next generation of researchers learned to self-censor.”
The U.S. dietary guidelines still recommend that we limit saturated fat and consume vegetable oils instead. They backed away from their caps on cholesterol in 2015 but issued no announcement to inform the public.
“This was one of the pillars of dietary advice for the last 60 years, and they dropped it by a single sentence in a nearly 400-page document without any explanation,” Teicholz said.
Teicholz explained that the U.S. dietary guidelines are enormously powerful since they serve as the backbone of our country’s nutrition policy. They dictate what is included in all federally-funded food programs, such as school lunches and military rations. They also are downloaded by healthcare professionals, societies, hospitals and clinics across the country, forming the basis of their dietary recommendations.
“The guidelines are a more powerful lever on what Americans eat than any other single document in the country,” Teicholz said.
Therefore, if any document should be based on the best possible evidence, devoid of all scientific and industry bias, it should be our dietary guidelines. However, experts say this is not the case.
“Unfortunately, the current and past U.S. dietary guidelines represent a nearly evidence-free zone,” writes Dr. Steven Nissen, chairman of cardiovascular medicine at the Cleveland Clinic in Ohio.
Experts like Nissen and Teicholz argue the guidelines are based on weak observational data, not high-quality randomized controlled trials that form the gold standard of scientific research.
“There is nothing evidence-based — that is, based on rigorous clinical trials — in the guidelines. It’s all based on weak epidemiological data, in many cases contradicted by more rigorous science,” Teicholz explained in an email.
Given that our top dietary recommendations are rooted in poor science, it is any wonder that our population is so unhealthy — and so confused about what to eat?
Part III: Missing the Mark in Treating Chronic Disease
Chronic diseases utterly overwhelm our medical system, accounting for 86 percent of healthcare spending. Sixty percent of adults have one chronic disease, while over 40 percent suffer from multiple conditions. Simply stating we have a chronic disease epidemic feels like an understatement.
Hold up. We live in the 21st century, an era of cutting-edge science and medicine. Shouldn’t we be able to stem the tide of illness? Why is the chronic disease epidemic just getting worse?
Quite simply, conventional medicine lacks the tools for the job.
The conventional medical framework looks something like this: you go to the doctor with a complaint. The doctor listens to your symptoms and prescribes a medication, usually within a 15-minute window.
“This is what we’re trained to do during medical school,” said Dr. Beth Frates, a Harvard Medical School professor and expert in lifestyle medicine. “It’s comfortable and reliable, and it’s what the patient is expecting.”

The problem is that while medications might help control the symptoms of chronic conditions, they do nothing to reverse their progress. Hence, chronic diseases — ranging from heart disease and diabetes to Alzheimer’s and cancer — account for 7 out of 10 deaths in our country.
This is a tragic state of affairs, given that these conditions are largely preventable. Frates said researchers debate what percentage of chronic diseases could be avoided, but she believes it falls somewhere around 80 percent.
“The number is debatable in terms of how much of chronic disease is preventable, but what is not debatable is that changing your lifestyle can treat — and in some cases, even reverse — your disease.”
This is an extraordinary concept, one that I didn’t believe myself when introduced to it for the first time. I thought that if we can truly prevent and even treat disease through lifestyle changes, surely more people would know about it. It took several months of sustained dialogue with a holistic practitioner for me to start shifting my rigid mindset, a mindset I had developed over 20 years of living a conventional American life.
To truly understand the power of lifestyle medicine, we need to take a brief look at the developing field of epigenetics. Epigenetics explains how environmental factors can influence gene expression and thus have profound implications for our health.
In other words, we are not merely our genetic code. We are the totality of our everyday life choices — from the realm of food and exercise to sleep and stress — that turn on or off our genes.
Frates says we must teach patients that their genes are not their destiny. Just because your parents had heart disease or diabetes does not mean you are doomed to the same fate. She believes doctors must explain the impact of our lifestyle choices and empower patients to take control over their health.
“We need to focus the majority of our attention on the possibility of beating disease with prescriptions for exercise, nutrition, sleep and stress management,” she said.
So why don’t doctors talk about lifestyle factors? There are a number of reasons, from lack of training and time to the very incentive structure of our healthcare system. Still, many doctors feel that patients simply don’t want to hear it.
“A lot of physicians don’t believe that patients will actually change. In my experience, many of them have a defeatist attitude, so they feel as though they’re wasting their time if they talk with patients about lifestyle,” said Todd Robinson, a naturopathic doctor and owner of Wellness Working Group.
Changing habits takes work. It’s much easier to pop a pill. At the end of my first neurology appointment, the doctor asked how I felt about being diagnosed with POTS. I said I felt fine…as long as there was a medication to take.
We live in a quick-fix culture, and sometimes the quick fixes appear to work. However, it has become clear that we cannot medicate our way out of the chronic disease epidemic.
Lifestyle medicine is not only more effective than conventional methods for treating many chronic diseases, it is also incredibly empowering. When I learned that I could take action to help me feel better, it was a turning point in my condition. I realized that I did not have to surrender my life to the whims of the doctor or the disease. I could take control.
“Clients feel empowered by natural medicine,” Robinson said. “That empowerment in and of itself is medicinal.”
But in order to successfully change their lifestyles, people need more guidance than a 15-minute appointment allows. It’s not enough for a doctor to say, “You need to work on your diet and incorporate some exercise and stress reduction into your day.” Most patients require a greater degree of support.
“The work I do with my clients has shown me that people need a lot more to effectively make changes. They need more information, more guidance, they need more ongoing support if there is going to be any real change,” Robinson said.
It is crucial to note that not all chronic diseases can be treated by lifestyle measures alone. Robinson, who specializes in cancer treatment, believes in an integrative approach that unites the best of both conventional and natural medicine. He explained that natural approaches are gentler and less potent than conventional treatments; therefore, stronger interventions are sometimes necessary. That being said, he does not want to minimize the impact of lifestyle on our health.
“I have seen people reduce or eliminate their need for some medications—for hypertension, diabetes, dyslipidemia, rheumatoid arthritis, etc.—through diet and lifestyle change,” Robinson said. “The impact of lifestyle on all disease is profound, even cancer.”
Frates says that most of the research on reversing chronic disease centers around diabetes and heart disease. While the data is less substantial for other conditions, many doctors describe patients dramatically improving after switching to a non-processed, whole foods diet.
“I cannot tell you how many stories I get from people who changed their diet and tell me their eczema has gone away, or their allergies have gone away, or their GI distress has gone away, or their irritable bowel has gone away,” Lustig said.
Now that we have a deeper understanding of why diet matters, let’s return to the world of processed food. What can we do to safeguard our wellbeing and ensure that we don’t wind up as just another chronic disease statistic?
In practical terms, the answer is simple: Eat real food. Banish as much processed food as you can from your kitchen. Learn to cook delicious meals from real ingredients, not those found in a package or box.
Yet while our individual choices yield tremendous power, it will take much more to fully transform our food environment. What about the countless Americans who do not have access to fresh fruits and vegetables? Or the children who never learned how to cook and so are — as Dr. Robert Lustig puts it — hostage to the food industry for their entire lives? Or the millions of individuals fed inaccurate nutrition advice thanks to bad science and bad journalism?
There have been many solutions tossed around the public health community: remove subsidies for commodity crops like soy and corn (and perhaps subsidize produce), regulate food marketing, tax sugary drinks, get junk food out of schools and hospitals, teach kids how to cook in home economics courses…and the list goes on.
In short, transforming our food environment will require a complete system-wide overhaul. It will require us to start prioritizing health over profit, placing long-term considerations over short-term gain. It will require doctors to start discussing food and patients to really listen. It will require that we return to our kitchens, rediscovering the joy of preparing wholesome meals for ourselves and our families.
But while all of these political and cultural considerations can threaten to overwhelm us with their complexity, we can take solace in the fact that we have power. We don’t have to wait for the government or industry or society to turn around. We can take control over our health each and everyday — with the basic decisions of what we eat for breakfast, lunch and dinner.
Original article was published here
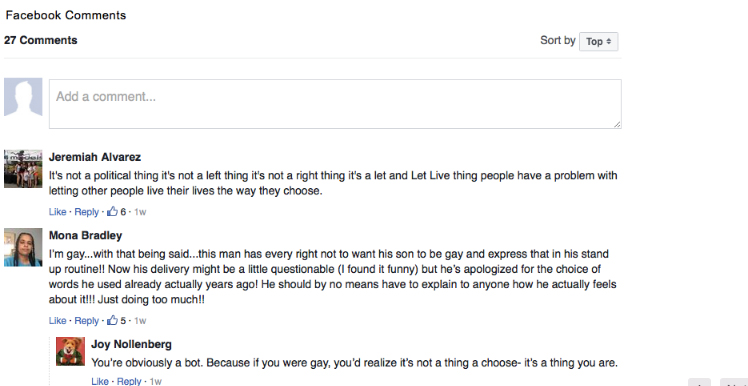



Facebook Comments